SESSION I: DRUG DISCOVERY 2.0
| Introduction and Welcome Notes | Howard Fillit, MD—Alzheimer’s Drug Discovery Foundation |
| SESSION I. DRUG DISCOVERY 2.0 | CHAIR: Walter Kostich, PhD—National Multiple Sclerosis Society |
| Omics to Identify Novel Target for Neurodegenerative Diseases | Philip De Jager, MD, PhD—Columbia University |
| Pre-clinical Science, Clinical Development and Pathway to Marketing Approval of a Living Cell Pharmaceutical for AD – the Mesenchymal Stem/Stromal Cell Paradigm | Jacques Galipeau, MD—University of Wisconsin, Madison |
| Shift in Medicinal Chemistry: from Organic Chemistry to Synthetic Biology | Edmund Graziani, PhD—Apertor Labs |
INTRODUCTION and WELCOME NOTES
Howard Fillit, MD
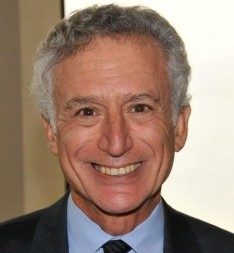 Howard Fillit, MD, is a geriatrician, neuroscientist, and innovative philanthropy executive, who has led the ADDF since its founding. Dr. Fillit has held faculty positions at The Rockefeller University, the SUNY-Stony Brook School of Medicine and the Cornell University School of Medicine. In 1987, he joined the Mount Sinai School of Medicine, where he is a clinical professor of geriatric medicine and palliative care, medicine and neuroscience. Dr. Fillit also maintains a limited private practice in consultative geriatric medicine with a focus on Alzheimer’s disease and related dementias.
Howard Fillit, MD, is a geriatrician, neuroscientist, and innovative philanthropy executive, who has led the ADDF since its founding. Dr. Fillit has held faculty positions at The Rockefeller University, the SUNY-Stony Brook School of Medicine and the Cornell University School of Medicine. In 1987, he joined the Mount Sinai School of Medicine, where he is a clinical professor of geriatric medicine and palliative care, medicine and neuroscience. Dr. Fillit also maintains a limited private practice in consultative geriatric medicine with a focus on Alzheimer’s disease and related dementias.
He has authored or co-authored more than 300 publications and is the senior editor of Brocklehurst’s Textbook of Geriatric Medicine and Gerontology. Dr. Fillit is the recipient of many awards and honors including the Rita Hayworth Award from the Alzheimer’s Association. He is a fellow of the American Geriatrics Society, the American College of Physicians, the Gerontological Society of America and the New York Academy of Medicine. Dr. Fillit earned his bachelor of arts in neurobiology cum laude from Cornell University and his medical degree from the SUNY-Upstate Medical University.
Session Overview
Walter Kostich, PhD - Chair, SESSION I
 Dr. Walter Kostich is the Director of Commercial Research at the National MS Society. He manages commercial research partnerships developed through the Fast Forward program. Fast Forward bridges the preclinical commercial funding gap by targeting funds to de-risk therapeutic development for MS. Walt also serves as a program officer for the academic research grant program, where he is responsible for grants with a clinical component.
Dr. Walter Kostich is the Director of Commercial Research at the National MS Society. He manages commercial research partnerships developed through the Fast Forward program. Fast Forward bridges the preclinical commercial funding gap by targeting funds to de-risk therapeutic development for MS. Walt also serves as a program officer for the academic research grant program, where he is responsible for grants with a clinical component.
A Neuroscientist by training, he joined the National MS Society in 2015 following a twenty-year career in the pharmaceutical industry in neuroscience drug discovery. He was most recently a Senior Research Investigator at Bristol-Myers Squibb. In that role he provided leadership for several preclinical drug discovery programs in neurologic and psychiatric disorders. Dr. Kostich earned a Masters degree from Washington University and a Doctoral degree from the University of Maryland.
Q&A
I was wondering if you could tell us more about funding opportunities for PhD and young investigators at your institution.
The National Multiple Sclerosis Society offers a spectrum of funding opportunities and other resources to support MS investigators at virtually every stage of their careers. For early Ph.D. investigators I would highlight three funding programs: Postdoctoral Fellowships, Career Transition Fellowships, and Pilot Grants. The Postdoctoral Fellowship program offers promising fellows up to 3 years of support to pursue MS-related, mentored research. The Career Transition Fellowship offers particularly promising postdoctoral trainees approximately $550,000 over five years to support a two-year period of advanced postdoctoral training in MS research and a bridge to the first three years of research in a new faculty appointment. Finally, many new faculty members take advantage of our Pilot grant program which provides up to $50,000 for one year to pursue innovative, cutting-edge ideas or untested methods and gather sufficient preliminary data to apply for longer-term funding.
The Society offers additional training opportunities for clinicians and clinician scientists and also longer term grant funding opportunities. For additional information on all of these programs and our research priorities please go to our website at: https://www.nationalmssociety.org/For-Professionals/Researchers/Society-Funding.
Omics to Identify Novel Targets for Neurodegenerative Diseases
Philip De Jager, MD, PhD—Columbia University
Philip De Jager, MD, PhD
 Dr. Philip De Jager is the Weil-Granat Professor of Neurology at Columbia University Medical Center, where he is the Chief of the Division of Neuroimmunology and directs the Center for Translational & Computational Neuroimmunology.
Dr. Philip De Jager is the Weil-Granat Professor of Neurology at Columbia University Medical Center, where he is the Chief of the Division of Neuroimmunology and directs the Center for Translational & Computational Neuroimmunology.
He graduated from Yale University (Molecular Biophysics & Biochemistry and Medieval French literature) and from the MD PhD program at Rockefeller University and Cornell University Medical College. He completed his neurology residency at Massachusetts General Hospital and Brigham and Women’s Hospital. His research program involves applying modern methods of human immunology, genomics, and computational biology to investigate neurodegenerative diseases such as AD, PD, and MS.
Q&A
Do you think that seasonal variation in the level of biomarkers should be implemented in clinical trials? If so, how?
Considering that there are groups of research and partnerships like AMP, do you think that it is still worth it for small labs to do their own research and unbiased (or biased) screening? There are such large datasets that I wonder what would be the added value.
What should I do to stay updated on the result of AMP? When can I see this results?
Can you clarify how your data analysis was performed? In particular, I’m wondering whether you included the circadian data and seasonality, or whether all data where collected all at the same time.
Does m109 correlates with Braak staging? Or more work needs to be done to evaluate individual proteins in this module?
I was wondering if you see differences in the extent of the seasonality effect in people who live in different regions of the world with more 'summer-like' days or vice-versa.
Do you have any data from the southern hemisphere? Is this seasonal variation opposite? Is there any research about "summer-like" elements and their impact on the cognitive decline? Like number of hours exposed to sunlight? Vitamin D levels, physical activity, etc?
It was amazing to see the cognitive performances changes associated with the seasons. One thing I did not see was if there were any differences in your analyses between men vs women? And also, do you believe particular brain regions/areas may end up having stronger effects in these 'omics responses (ie. can we establish that timeline you showed as initiating in one brain region and then driving the rest of the CNS with it)?
Pre-clinical Science, Clinical Development and Pathway to Marketing Approval of a Living Cell Pharmaceutical for AD – the Mesenchymal Stem/Stromal Cell Paradigm
Jacques Galipeau, MD—University of Wisconsin, Madison
Jacques Galipeau, MD
 Dr. Jacques Galipeau is the Don and Marilyn Anderson Professor of Oncology within the Department of Medicine and UW Carbone Comprehensive Cancer Center at the University of Wisconsin in Madison, and is Associate Dean for Therapeutics Development at the University of Wisconsin School of Medicine & Public Health. He is the director of the University of Wisconsin Advanced Cell Therapy Program whose mission is to develop personalized cell therapies for immune and malignant disorders and to promote and deploy first-in-human clinical trials of UW cell therapy innovations to improve outcomes for children and adults.
Dr. Jacques Galipeau is the Don and Marilyn Anderson Professor of Oncology within the Department of Medicine and UW Carbone Comprehensive Cancer Center at the University of Wisconsin in Madison, and is Associate Dean for Therapeutics Development at the University of Wisconsin School of Medicine & Public Health. He is the director of the University of Wisconsin Advanced Cell Therapy Program whose mission is to develop personalized cell therapies for immune and malignant disorders and to promote and deploy first-in-human clinical trials of UW cell therapy innovations to improve outcomes for children and adults.
Dr. Galipeau leads a research program in the study and use of mesenchymal stromal cells as an immunotherapy of catastrophic illnesses including cancer and immune disease. He has also developed the field of fusion engineered cytokines known as fusokines, as a novel pharmaceutical means of treating immune disorders and cancer. He is an internationally recognized expert in translational development of cellular pharmaceuticals and the sponsor of a series of FDA-sanctioned clinical trials examining the use of personalized cell therapies.
Dr. Galipeau is the Chair of the ISCT MSC Committee.
Q&A
You showed that in about a month you can generate a kilo of cells. In view of clinical applications, would the “production” of these cells be so simple? Or different, maybe more strict, conditions will be required to be sure that every batch would be the same?
1) How would you measure target engagement in a clinical trials using MSC in a neurodegenerative disease? How can we measure their effectiveness? 2. Lots of trials have been done using stem cells, and many in neurodegenerative disease. You mentioned that only 1 out of 914 trials got approval, do you know what they used in that trial as measure of target engagement?
Do you think that research on excipients, nanoparticle, delivery system, membrane stabilizers etc. could increase the stability of MSC and other stem cell lines so that they could be frozen/thawed?
Which kind of preclinical stem cell research is still needed? Or, at this point, we are ready to focus 100% on clinical studies?
In your very last slide you mentioned predictive biomarkers of response. Could you elaborate this a bit more, and let us know what do we know today?
I wonder whether administration of MSCs for neurodegeneration will depend on disease stage or be most effective for diseases with clear neuro-inflammatory component? Eg will neuroinflammation need to be present for these treatments to be effective rather than given prophylactically?
Is there a risk of tumourigenesis with administering MSCs that develop to M2-like macrophages?
Medicinal Synthetic Biology in Drug Discovery
Edmund Graziani, PhD—Apertor Labs
Edmund Graziani, PhD
 Dr. Edmund Graziani is a natural products chemist with 20 years’ experience in drug discovery at Wyeth and Pfizer, where he was Research Fellow. His research contributions have included the discovery of novel leads for early phase programs in oncology, as well as the discovery of ILS-920, a non-immunosuppressive analog of the mTORC1 allosteric inhibitor rapamycin (sirolimus). ILS-920 entered Phase 1 clinical trials for amelioration of neurological deficits following ischemic stroke in 2009.
Dr. Edmund Graziani is a natural products chemist with 20 years’ experience in drug discovery at Wyeth and Pfizer, where he was Research Fellow. His research contributions have included the discovery of novel leads for early phase programs in oncology, as well as the discovery of ILS-920, a non-immunosuppressive analog of the mTORC1 allosteric inhibitor rapamycin (sirolimus). ILS-920 entered Phase 1 clinical trials for amelioration of neurological deficits following ischemic stroke in 2009.
At Pfizer, Dr. Graziani established a bioconjugation chemistry group that contributed to the discovery of novel antibody-drug conjugates resulting in multiple clinical candidates for oncology indications. He is currently CEO and co-founder with Prof. Jay Keasling of Apertor Labs, a synthetic biology start-up focused on the discovery of novel reversible allosteric inhibitors of mTORC1 for treating diseases of the aging immune system.
Q&A
Which kind of patent can you obtain using synthetic biology?
How, in your opinion, can a postdoc or a PI design clever experiments to avoid testing a large number of natural product in animal model?
EG: This is an important question, thanks! Ideally, you would decide upon specific in vitro criteria that you think are most predictive of a pharmacologic response in your animal model, and then obtain and use those data to triage compounds for pharmacokinetic studies prior to testing in an animal model.
If natural products have so many potential great properties and allow to explore a chemical space that traditional chemistry does not allow, why big Pharma is not investing in this space?
EG: While it is true that natural products are often cyclical in terms of interest from industry, and the larger pharmaceutical companies in particular, there are still large pharmaceutical companies that work on natural products (i.e. Novartis). But I certainly agree that natural products SHOULD continue to be substrate for clinical development from companies large and small!
Your last slide would require an entire talk, or maybe meeting, to be discussed. Could you elaborate more on some of the outstanding questions that your company is trying to address, and some of the challenges that you are facing?
EG: Thank-you, and you’re right that I threw out some deliberately provocative and challenging questions for the field. One of the biggest challenges is working with wild-type organisms and the associated challenges of engineering good heterologous hosts for expression of complex macrocycles, for example. I hope we will begin to see more discussion on these subjects.
How many companies, that you are aware of, are using synthetic biology to create new molecules? In other words, is this a crowded space?
EG: I can’t hazard an exact number, but the number of companies using synthetic biology for pharmaceuticals is certainly growing.
Do you intend to use the PKS/NRPS systems to generate a library of previously unknown natural products and to then screen them using an HTS pipeline?
EG: What I proposed in the workshop was a thought experiment, as there are substantial challenges that remain in order to begin to build such a system. But, yes, in theory, if one could engineer such a system, that would be the plan!
What do you think it would take see the enthusiasm for natural product starting materials in academic or pharmaceutical neuroscience drug discovery efforts? As you pointed out, some of the most lifesaving drugs to date are isolated natural compounds so you would think this would have become a more common approach. Also, could you point me in the direction of groups or companies that are currently leading discovery efforts with natural product-derived drugs? Your idea to systematically alter the enzymes responsible for creating these natural molecules and couple to a high throughput (yeast) reporter system is very elegant and hopefully extremely powerful. Inspiring!
EG: Thank you! I think the best way to increase interest in this approach is to (re)demonstrate that it works! That is to say, if smaller companies can use this or related approaches to bring new natural product-based therapies to the clinic, then others will follow.
